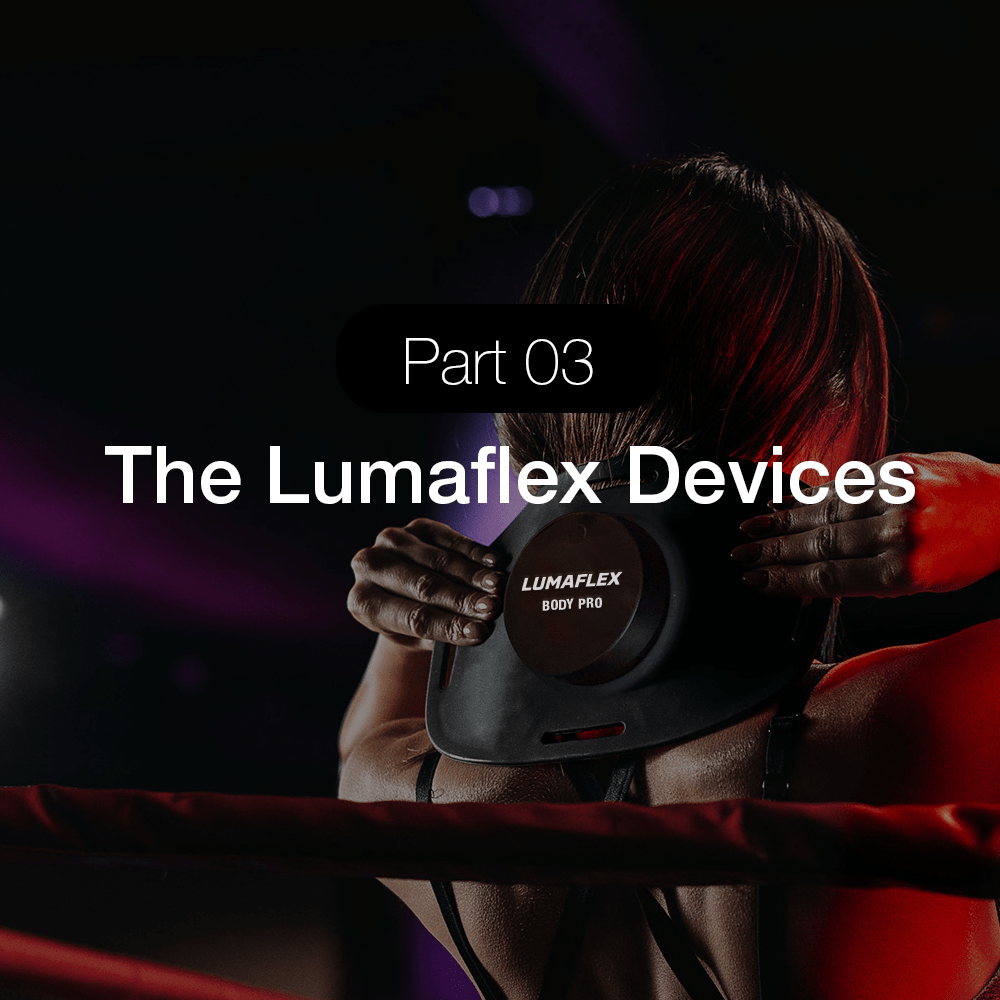
A Meta-analysis: Red Light Therapy for Depression Treatment

Red light therapy, also known as photobiomodulation (PBM) or low-level laser therapy, represents a promising non-invasive treatment for major depressive disorder with growing clinical evidence and well-characterized biological mechanisms. Current research demonstrates moderate therapeutic efficacy comparable to established antidepressant treatments, with superior safety profiles and faster onset of action than conventional pharmacotherapy.
Table of content
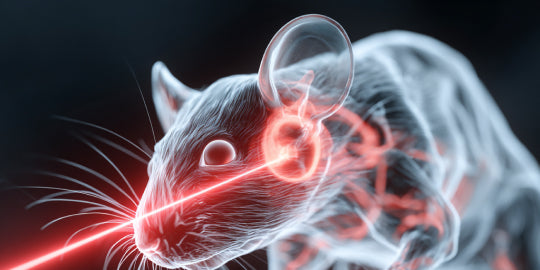
Mechanisms of Action
Red light therapy operates through multiple interconnected biological pathways that address the complex pathophysiology of depression. The primary mechanism centers on cytochrome c oxidase (Complex IV) in the mitochondrial respiratory chain, which serves as the key photoacceptor for therapeutic wavelengths (810-830 nm). Light absorption dissociates inhibitory nitric oxide from cytochrome c oxidase, enhancing electron transport and increasing cellular ATP production by up to 200% through optimized oxidative phosphorylation.
Neurobiological effects drive therapeutic outcomes
The therapy promotes neuroplasticity through multiple pathways, including enhanced brain-derived neurotrophic factor (BDNF) expression via CREB activation. Clinical studies demonstrate significant BDNF increases (delta values of 821.94 vs 359.41 treatment vs placebo) correlating with improved mood outcomes. Neurogenesis stimulation occurs particularly in the hippocampus, with enhanced proliferation of neural progenitor cells and improved integration of newborn neurons into existing circuits.
Red light therapy modulates key neurotransmitter systems implicated in depression, including increased serotonin synthesis and availability, enhanced dopamine transporter expression, and normalized glutamate levels through improved GLT-1 transporter function. The therapy also demonstrates potent anti-inflammatory effects, reducing pro-inflammatory cytokines (IL-1β, IL-6, TNF-α) while enhancing anti-inflammatory mediators like IL-10.
Brain-specific targeting enhances clinical relevance
Transcranial applications preferentially target the prefrontal cortex and limbic structures critical for mood regulation. The therapy increases regional cerebral blood flow, enhances glucose utilization, and normalizes dysfunctional brain networks including the default mode network commonly altered in depression. Circadian rhythm modulation through both direct neural pathways and systemic effects contributes to improved sleep architecture and seasonal depression treatment.
Clinical Studies and Evidence Base
The clinical evidence for red light therapy in depression has expanded significantly, with multiple systematic reviews and meta-analyses demonstrating consistent therapeutic benefits. The most comprehensive meta-analysis by Ji et al. (2024) included 11 randomized controlled trials with 407 participants, finding significant reduction in depression symptoms (SMD = -0.55, 95% CI [-0.75, -0.35]) with moderate effect sizes.
Landmark clinical trials establish efficacy
The ELATED trial series represents the most rigorous clinical evidence, with ELATED-2 (2018) demonstrating significant improvements in Hamilton Depression Rating Scale scores using 823 nm near-infrared light applied transcranially. The multicenter ELATED-3 trial (2022) confirmed antidepressant effects using very low-level transcranial photobiomodulation protocols. Response rates consistently range from 40-89% across studies, with some trials reporting remission rates up to 89%.
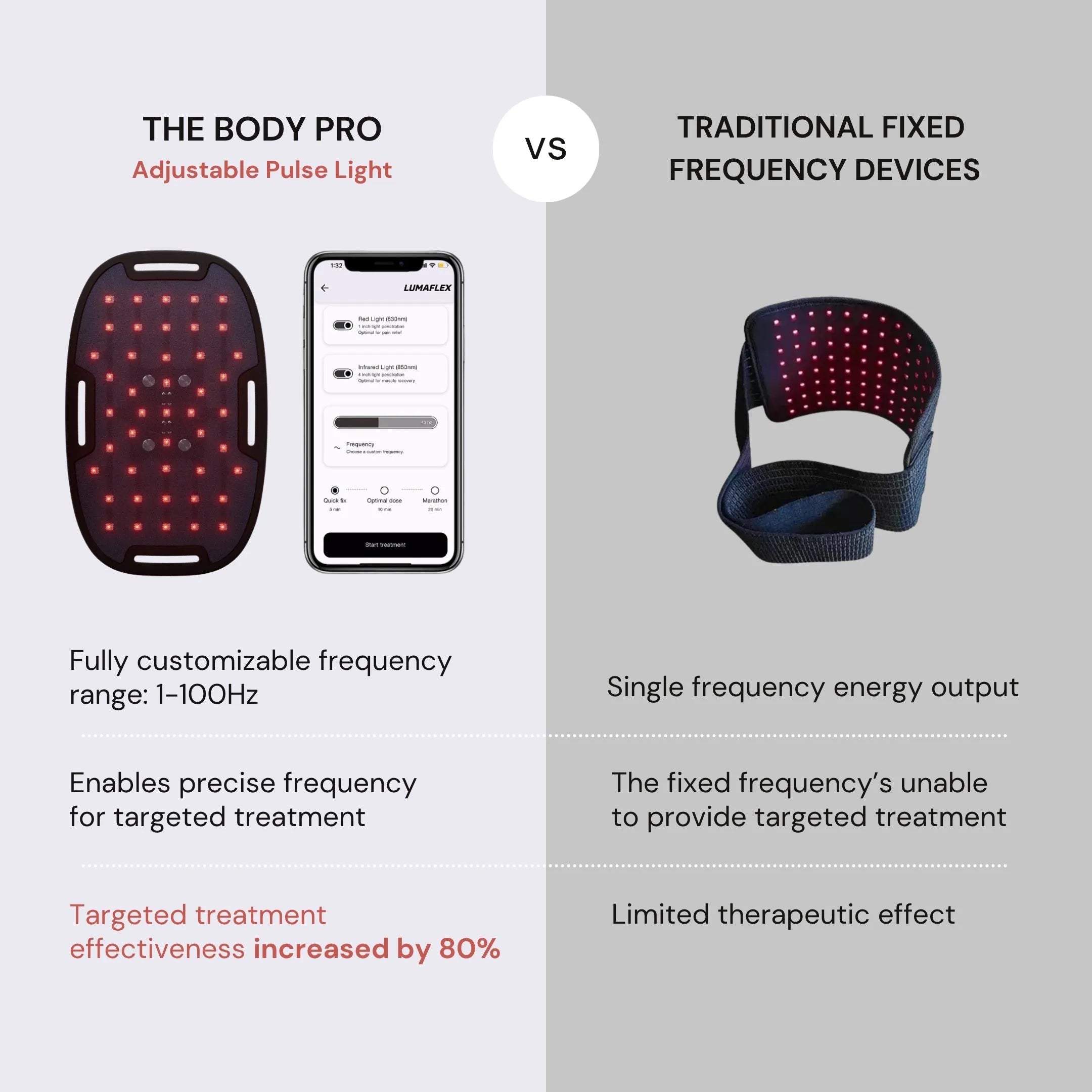
Recent research has focused on optimizing treatment parameters, with studies identifying wavelengths of 808-823 nm as most effective for depression. The optimal transcranial protocol involves 823 nm wavelength, 36-50 mW/cm² power density, applied for 20-30 minutes, 2-3 times weekly for at least 15 sessions targeting the dorsolateral prefrontal cortex bilaterally.
Treatment protocols continue evolving
Emerging evidence suggests full-body systemic approaches may complement transcranial protocols, with systemic PBM using 808 nm wavelength, 50-100 mW/cm² power density, applied for 5 minutes, 3+ times weekly showing additional benefits. Wearable device applications demonstrate good safety and compliance profiles, enabling home-based treatment delivery.
Efficacy and Comparative Effectiveness
Red light therapy demonstrates comparable efficacy to established depression treatments with several unique advantages. Meta-analytic evidence shows 41% remission rates versus 23.5% with other treatments (p < 0.001), with Harvard Medical School research confirming effectiveness "approximately the same as antidepressant medications" achieving 40-60% symptom improvement rates.
Response characteristics favor rapid onset
The therapy shows significantly faster onset than antidepressants, with improvements typically observed within one week compared to 4-6 weeks required for full pharmacological effects. Some studies demonstrate immediate mood improvements within one hour of treatment, representing a major clinical advantage for acute depression management.
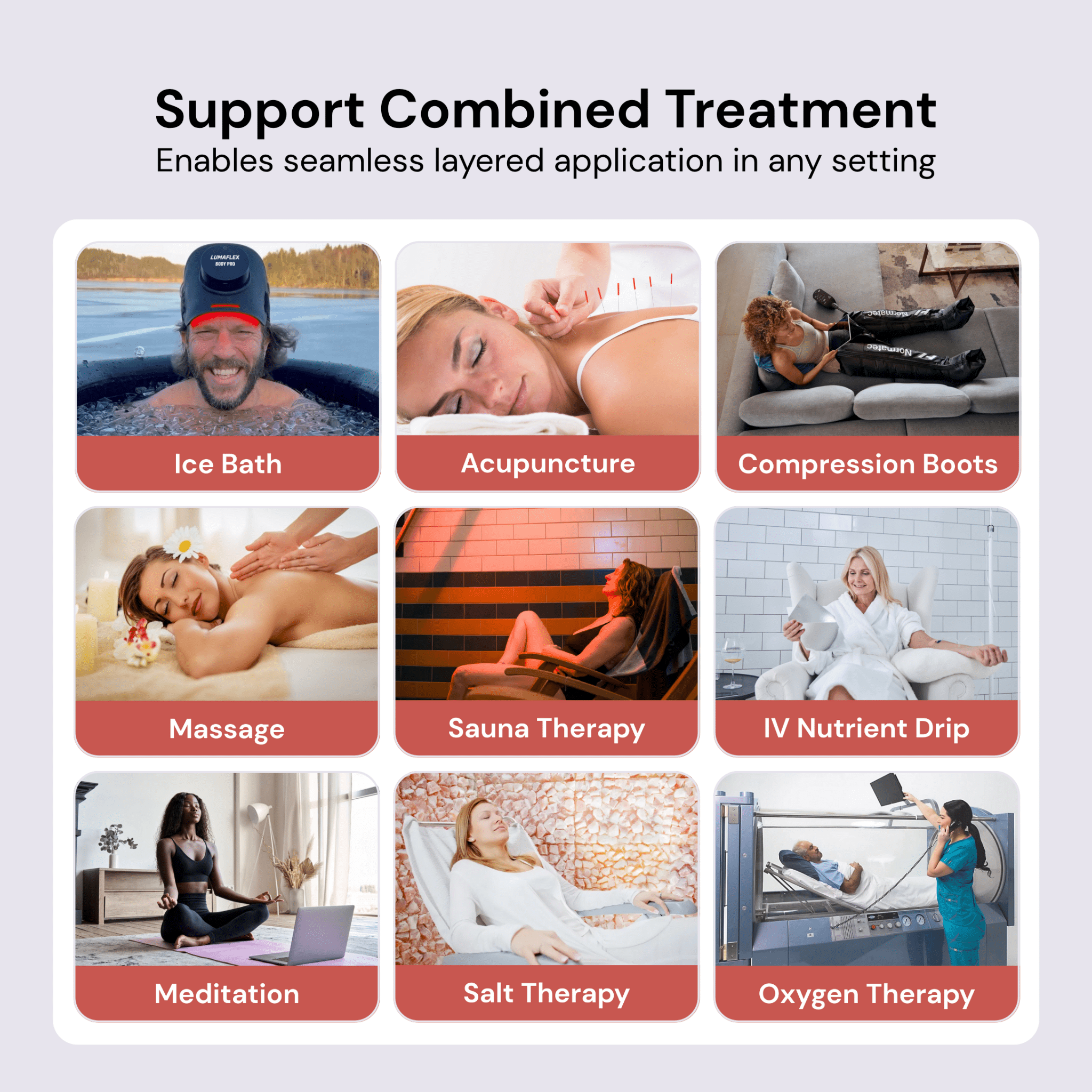
Combination therapy approaches demonstrate superior outcomes, with light therapy plus antidepressants significantly outperforming monotherapy (SMD = 0.56, p < 0.001). This synergistic effect positions red light therapy as an effective augmentation strategy rather than replacement for conventional treatments.
Durability and maintenance considerations
While acute effects are well-documented, long-term durability data remains limited. Available studies suggest effects maintain for 2-4 weeks post-treatment, with some patients showing sustained benefits up to 55 months. Optimal maintenance protocols are still under investigation, though regular "booster" treatments may extend durability.
Safety Profile and Clinical Applications
Red light therapy demonstrates an exceptionally favorable safety profile with minimal adverse events reported across clinical trials. The most commonly reported side effects include mild headaches, transient fatigue, and localized skin warming, affecting fewer than 5% of patients. No serious adverse events have been reported in depression-focused clinical trials.
Contraindications are limited but important
Absolute contraindications include active malignancy (theoretical risk of stimulating cancer cell proliferation), pregnancy (unknown fetal effects), photosensitizing medications, and photosensitivity disorders. Relative contraindications include hyperthyroidism when applied to neck area, recent eye surgery, seizure disorders, and implanted medical devices requiring physician consultation.
The therapy shows superior tolerability compared to antidepressants, which have 42% discontinuation rates within 30 days due to adverse events. This favorable profile makes red light therapy particularly valuable for elderly patients, those with medical comorbidities, and patients intolerant of conventional treatments.
Current regulatory status and quality standards
While no specific FDA approval exists for depression treatment, devices receive FDA clearance as Class II medical devices for general wellness applications. Quality standards require IEC 60601 compliance for medical-grade safety, with proper certification including ETL/UL listing, CE marking, and FCC compliance essential for clinical applications.
Current clinical practice guidelines recommend medical supervision for depression treatment, comprehensive assessment to rule out contraindications, integration with standard depression treatments, and systematic monitoring of response and side effects.
Treatment Protocols and Clinical Implementation
Evidence-based protocols have emerged from systematic research, with transcranial photobiomodulation requiring specific parameters for optimal efficacy. The gold standard protocol uses 823 nm wavelength, applied at 36-50 mW/cm² power density for 30-minute sessions, delivered 2-3 times weekly targeting bilateral dorsolateral prefrontal cortex.
Energy density parameters of 10-100 J/cm² demonstrate superior outcomes compared to higher densities, suggesting a biphasic dose-response relationship where excessive treatment reduces efficacy. Treatment duration exceeding 15 sessions consistently shows better outcomes than shorter protocols.
Device specifications ensure therapeutic efficacy
Critical device requirements include wavelength accuracy verification, power output stability, irradiance uniformity, temperature monitoring, timer controls, and eye protection features. Quality manufacturing standards must include ISO 13485 medical device quality management, Good Manufacturing Practice compliance, third-party testing, and calibration certificates.
Professional training recommendations emphasize proper device selection, dosimetry documentation, gradual dose escalation starting with lower parameters, and integration with comprehensive depression care including psychiatric oversight for severe cases.
Research Limitations and Gaps
Despite promising evidence, significant methodological limitations constrain definitive clinical recommendations. AMSTAR-2 evaluations found 5 of 6 systematic reviews rated as "critically low quality," with most individual studies involving small sample sizes (20-50 participants) and significant heterogeneity in protocols, populations, and outcomes.
Critical research gaps require attention
Standardization represents the most significant gap, with lack of consensus on optimal wavelengths, intensities, duration, and frequency parameters. Long-term follow-up data remains limited, with most studies providing outcomes only through 8-12 weeks post-treatment. Mechanism clarity requires further investigation, particularly regarding dose-response relationships and individual variability in treatment response.
Methodological improvements needed include larger sample sizes (>100 participants per arm), rigorous blinding procedures with appropriate controls, standardized outcome measures, and multi-site collaboration for enhanced generalizability. Population-specific research is particularly lacking for adolescents, elderly patients, and treatment-resistant depression.
Evidence quality assessment reveals mixed findings
Current GRADE evidence quality ratings range from moderate for depression outcomes to very low for sleep outcomes, reflecting the heterogeneity and methodological limitations across studies. Only 13% of light therapy studies in early systematic reviews met rigorous inclusion criteria, indicating substantial room for methodological improvement.
Future Research Directions
Priority research areas focus on addressing current limitations through large-scale, multicenter randomized controlled trials with standardized protocols and long-term follow-up. Mechanistic research should investigate mitochondrial function effects, neuroplasticity markers, circadian regulation mechanisms, and inflammation modulation pathways.
Emerging applications show promise
Combination therapy protocols represent a high-priority research area, particularly photobiomodulation combined with cognitive behavioral therapy, sleep hygiene interventions, and precision medicine approaches based on biomarkers. Technology advances in wearable, self-administered devices enable home treatment delivery and real-time monitoring with adaptive protocols.
Novel applications under investigation include prevention of depression relapse, treatment of subsyndromal depression, cognitive enhancement in depression, and inflammation-targeted protocols. Biomarker development research focuses on inflammatory markers, neurotrophic factors, and neuroimaging correlates as treatment response predictors.
Personalized medicine approaches should investigate genetic, demographic, and clinical factors predicting treatment response, enabling optimized individualized protocols. Cost-effectiveness analyses will be crucial for healthcare implementation and insurance coverage decisions.
Conclusion
Red light therapy for depression treatment demonstrates compelling therapeutic potential supported by well-characterized biological mechanisms and growing clinical evidence. The therapy offers unique advantages including rapid onset of action, excellent safety profile, potential for self-administration, and enhanced outcomes when combined with conventional treatments.
Current evidence supports red light therapy as a viable first-line or adjunctive treatment for depression, particularly given its favorable risk-benefit profile. However, larger randomized controlled trials with standardized protocols are essential to establish definitive clinical guidelines and optimize treatment parameters.
The convergence of cellular energy enhancement, neuroplasticity promotion, brain circuit modulation, circadian regulation, and anti-inflammatory effects provides a comprehensive therapeutic framework addressing depression's complex pathophysiology. As research continues to address methodological limitations and optimize treatment protocols, red light therapy appears positioned to become an important component of comprehensive depression care.
Future success will depend on coordinated research efforts prioritizing standardization, larger trial designs, mechanistic clarification, and personalized treatment optimization. The therapy's non-invasive nature, minimal side effects, and potential for widespread accessibility make it particularly valuable for addressing the global burden of depression across diverse populations and healthcare settings.
References
- Ji Q, Yan S, Ding J, Zeng X, Liu Z, Zhou T, Wu Z, Wei W, Li H, Liu S, Ai S. Photobiomodulation improves depression symptoms: a systematic review and meta-analysis of randomized controlled trials. Front Psychiatry. 2024 Jan 31;14:1267415. doi: 10.3389/fpsyt.2023.1267415. PMID: 38356614; PMCID: PMC10866010.
- Wang L, Mao L, Huang Z, Switzer JA, Hess DC, Zhang Q. Photobiomodulation: shining a light on depression. Theranostics. 2025 Jan 1;15(2):362-383. doi: 10.7150/thno.104502. PMID: 39744683; PMCID: PMC11671386.
- Cassano P, Petrie SR, Mischoulon D, Cusin C, Katnani H, Yeung A, De Taboada L, Archibald A, Bui E, Baer L, Chang T, Chen J, Pedrelli P, Fisher L, Farabaugh A, Hamblin MR, Alpert JE, Fava M, Iosifescu DV. Transcranial Photobiomodulation for the Treatment of Major Depressive Disorder. The ELATED-2 Pilot Trial. Photomed Laser Surg. 2018 Dec;36(12):634-646. doi: 10.1089/pho.2018.4490. Epub 2018 Oct 20. PMID: 30346890; PMCID: PMC7864111.
- Nairuz T, Sangwoo-Cho, Lee JH. Photobiomodulation Therapy on Brain: Pioneering an Innovative Approach to Revolutionize Cognitive Dynamics. Cells. 2024 Jun 3;13(11):966. doi: 10.3390/cells13110966. PMID: 38891098; PMCID: PMC11171912.
- Tafur J, Mills PJ. Low-intensity light therapy: exploring the role of redox mechanisms. Photomed Laser Surg. 2008 Aug;26(4):323-8. doi: 10.1089/pho.2007.2184. PMID: 18665762; PMCID: PMC2996814.
- de Oliveira BH, Lins EF, Kunde NF, Salgado ASI, Martins LM, Bobinski F, Vieira WF, Cassano P, Quialheiro A, Martins DF. Transcranial photobiomodulation increases cognition and serum BDNF levels in adults over 50 years: A randomized, double-blind, placebo-controlled trial. J Photochem Photobiol B. 2024 Nov;260:113041. doi: 10.1016/j.jphotobiol.2024.113041. Epub 2024 Oct 5. PMID: 39423445.
- Chang, S.-Y.; Lee, M.Y. Photobiomodulation of Neurogenesis through the Enhancement of Stem Cell and Neural Progenitor Differentiation in the Central and Peripheral Nervous Systems. Int. J. Mol. Sci. 2023, 24, 15427. https://doi.org/10.3390/ijms242015427
- Heo, JC., Park, JA., Kim, DK. et al. Photobiomodulation (660 nm) therapy reduces oxidative stress and induces BDNF expression in the hippocampus. Sci Rep 9, 10114 (2019). https://doi.org/10.1038/s41598-019-46490-4
- Shamloo S, Defensor E, Ciari P, Ogawa G, Vidano L, Lin JS, Fortkort JA, Shamloo M, Barron AE. The anti-inflammatory effects of photobiomodulation are mediated by cytokines: Evidence from a mouse model of inflammation. Front Neurosci. 2023 Apr 6;17:1150156. doi: 10.3389/fnins.2023.1150156. PMID: 37090796; PMCID: PMC10115964.
- Hao W, Dai X, Wei M, Li S, Peng M, Xue Q, Lin H, Wang H, Song P, Wang Y. Efficacy of transcranial photobiomodulation in the treatment for major depressive disorder: A TMS-EEG and pilot study. Photodermatol Photoimmunol Photomed. 2024 Mar;40(2):e12957. doi: 10.1111/phpp.12957. PMID: 38470033.
- Ma H, Du Y, Xie D, Wei ZZ, Pan Y, Zhang Y. Recent advances in light energy biotherapeutic strategies with photobiomodulation on central nervous system disorders. Brain Res. 2024 Jan 1;1822:148615. doi: 10.1016/j.brainres.2023.148615. Epub 2023 Oct 14. PMID: 37783261.
- Askalsky P, Iosifescu DV. Transcranial Photobiomodulation For The Management Of Depression: Current Perspectives. Neuropsychiatr Dis Treat. 2019 Nov 22;15:3255-3272. doi: 10.2147/NDT.S188906. PMID: 31819453; PMCID: PMC6878920.
- Perera S, Eisen R, Bhatt M, Bhatnagar N, de Souza R, Thabane L, Samaan Z. Light therapy for non-seasonal depression: systematic review and meta-analysis. BJPsych Open. 2016 Mar 4;2(2):116-126. doi: 10.1192/bjpo.bp.115.001610. PMID: 27703764; PMCID: PMC4998929.
- Gutiérrez-Menéndez A, Marcos-Nistal M, Méndez M, Arias JL. Photobiomodulation as a promising new tool in the management of psychological disorders: A systematic review. Neurosci Biobehav Rev. 2020 Dec;119:242-254. doi: 10.1016/j.neubiorev.2020.10.002. Epub 2020 Oct 15. PMID: 33069687.
- Vieira, Willians & Iosifescu, Dan & McEachern, Kayla & Gersten, Maia & Cassano, Paolo. (2023). Photobiomodulation: An Emerging Treatment Modality for Depression. 10.1016/j.psc.2023.02.013.
- Ta-Wei Guu, Paolo Cassano, Wan-Jing Li, Yu-Hsiung Tseng, Wen-Yu Ho, Yi-Ting Lin, Sheng-Yu Lin, Jane Pei-Chen Chang, David Mischoulon, Kuan-Pin Su, Wearable, self-administered transcranial photobiomodulation for major depressive disorder and sleep: A randomized, double blind, sham-controlled trial, Journal of Affective Disorders, Volume 372, 2025, Pages 635-642, ISSN 0165-0327, https://doi.org/10.1016/j.jad.2024.12.065.
- Flora J, Watson Huffer K. Transcranial Photobiomodulation Therapy as an Intervention for Opioid Cravings and Depression: A Pilot Cohort Study. Photobiomodul Photomed Laser Surg. 2024 Aug;42(8):509-513. doi: 10.1089/photob.2024.0032. Epub 2024 Aug 7. PMID: 39110620.
- Reeves GM, Nijjar GV, Langenberg P, Johnson MA, Khabazghazvini B, Sleemi A, Vaswani D, Lapidus M, Manalai P, Tariq M, Acharya M, Cabassa J, Snitker S, Postolache TT. Improvement in depression scores after 1 hour of light therapy treatment in patients with seasonal affective disorder. J Nerv Ment Dis. 2012 Jan;200(1):51-5. doi: 10.1097/NMD.0b013e31823e56ca. PMID: 22210362; PMCID: PMC5336550.
- Naeser MA, Zafonte R, Krengel MH, Martin PI, Frazier J, Hamblin MR, Knight JA, Meehan WP 3rd, Baker EH. Significant improvements in cognitive performance post-transcranial, red/near-infrared light-emitting diode treatments in chronic, mild traumatic brain injury: open-protocol study. J Neurotrauma. 2014 Jun 1;31(11):1008-17. doi: 10.1089/neu.2013.3244. Epub 2014 May 8. PMID: 24568233; PMCID: PMC4043367.
- Geoffroy PA, Schroder CM, Reynaud E, Bourgin P. Efficacy of light therapy versus antidepressant drugs, and of the combination versus monotherapy, in major depressive episodes: A systematic review and meta-analysis. Sleep Med Rev. 2019 Dec;48:101213. doi: 10.1016/j.smrv.2019.101213. Epub 2019 Sep 18. PMID: 31600678.
- Tao L, Jiang R, Zhang K, Qian Z, Chen P, Lv Y, Yao Y. Light therapy in non-seasonal depression: An update meta-analysis. Psychiatry Res. 2020 Sep;291:113247. doi: 10.1016/j.psychres.2020.113247. Epub 2020 Jun 22. PMID: 32622169.
- Salehpour F, Rasta SH. The potential of transcranial photobiomodulation therapy for treatment of major depressive disorder. Rev Neurosci. 2017 May 24;28(4):441-453. doi: 10.1515/revneuro-2016-0087. PMID: 28231069.
- Vieira WF, Gersten M, Caldieraro MAK, Cassano P. Photobiomodulation for Major Depressive Disorder: Linking Transcranial Infrared Light, Biophotons and Oxidative Stress. Harv Rev Psychiatry. 2023 May-Jun 01;31(3):124-141. doi: 10.1097/HRP.0000000000000363. PMID: 37171473.
- Cassano P, Petrie SR, Hamblin MR, Henderson TA, Iosifescu DV. Review of transcranial photobiomodulation for major depressive disorder: targeting brain metabolism, inflammation, oxidative stress, and neurogenesis. Neurophotonics. 2016 Jul;3(3):031404. doi: 10.1117/1.NPh.3.3.031404. Epub 2016 Mar 4. PMID: 26989758; PMCID: PMC4777909.
- Dong C, Shi H, Liu P, Si G, Yan Z. A critical overview of systematic reviews and meta-analyses of light therapy for non-seasonal depression. Psychiatry Res. 2022 Aug;314:114686. doi: 10.1016/j.psychres.2022.114686. Epub 2022 Jun 21. PMID: 35753223.