Scalp Psoriasis and Psoriatic Arthritis Diet: Healing Foods vs. Triggers

Introduction
If you’re living with both scalp psoriasis and psoriatic arthritis, you already know how tough the double challenge can feel. The itching and flaking scalp alone is exhausting, and when you add stiff, painful joints on top of it, even simple daily routines can feel overwhelming. You are not alone. In the United States, about 8 million people have psoriasis, and nearly one in three develop psoriatic arthritis. On top of that, more than half of people with psoriasis experience scalp involvement.
The link between these conditions is chronic inflammation. When your immune system gets stuck in “overdrive,” it does not just cause red, scaly patches on your scalp. It also sends signals that lead to swollen, achy joints.
Here is the good news: while medical care is essential, your diet can make a big difference. Certain foods fuel inflammation, while others calm it down and support healing from the inside out.
In this guide, you will discover how to:
- Spot common food triggers that can make symptoms worse
- Build a healing diet with skin and joint-friendly foods
- Pair nutrition with complementary care like red light therapy for better results
Think of it as your evidence-based and practical roadmap to feeling more in control of your body again.
Table of contents
Understanding the Connection Between Scalp Psoriasis and Psoriatic Arthritis
If you have scalp psoriasis and joint pain, it might feel like you are dealing with two completely separate problems. In reality, they are closely linked. Both conditions are part of psoriatic disease, which is an autoimmune disorder. That means your immune system mistakenly attacks healthy cells instead of protecting them.
This attack sets off systemic inflammation , which spreads through your whole body. On the outside, that can show up as itchy, flaky patches on your scalp. On the inside, it can cause swelling, stiffness, and discomfort in your joints. Many people who start with scalp psoriasis eventually develop psoriatic arthritis because of this shared inflammatory pathway.
Here is where your diet matters. Every meal you eat can either add fuel to this inflammation or help reduce it. Inflammatory foods like refined sugar and fried items can make symptoms flare, while nutrient-rich foods such as colorful vegetables and omega-3 fatty fish can support an anti-inflammatory response. By paying attention to what goes on your plate, you can directly influence how your skin and joints feel. This makes diet a powerful tool for managing psoriatic disease from the inside out.

The Science Behind Food and Inflammation in Psoriatic Disease
The food you eat has a direct impact on how your body handles inflammation. Some foods can trigger an immune reaction that raises levels of inflammatory markers such as TNF-alpha and IL-6. These markers signal your immune system to release cytokines, which act like chemical messengers spreading inflammation throughout the body.
When this happens, the effects can show up in different ways. Your skin may react with faster cell turnover, leading to thick, scaly patches. Your joints may respond with swelling, stiffness, or pain.
The good news is that by noticing how your body responds to different foods, you can begin to make choices that lower these signals. Over time, shifting toward an anti-inflammatory diet can reduce flare-ups, support joint comfort, and give your skin a chance to heal more effectively.
Foods That Trigger Scalp Psoriasis and Psoriatic Arthritis Flares
When you are living with scalp psoriasis and psoriatic arthritis, some foods can quietly fuel the fire of inflammation. These are often called trigger foods, and they can make flare-ups more frequent or more intense. By learning which foods are most likely to cause problems, you can start swapping them out for better options that calm your system instead of aggravating it.

Refined Sugars and Processed Foods That Worsen Psoriasis
Sugar is one of the biggest culprits when it comes to inflammation. Eating too much refined sugar can spike your blood sugar, which pushes your body to release more inflammatory chemicals. For people with psoriatic disease, this can mean more scalp irritation and stiffer joints. Processed foods are just as problematic since they often contain hidden sugars and unhealthy fats.
Foods to limit:
- Sugary drinks such as soda, sweetened teas, or flavored coffee
- Pastries, cookies, candy, and other sweets
- White bread and packaged snack foods
Better choices:
- Naturally sweet foods like fruit, dates, or unsweetened applesauce
- Small amounts of natural sweeteners such as raw honey, maple syrup, or monk fruit extract
- Whole, minimally processed snacks like nuts or fresh veggies
Gluten and Wheat as Common Trigger Foods in Psoriatic Arthritis
For some people, gluten can be a trigger that makes skin flares and joint pain worse. Research suggests that even without celiac disease, people with psoriatic disease may react poorly to gluten. The tricky part is that gluten hides in many everyday foods.
Hidden sources of gluten include:
- Soy sauce (try tamari instead)
- Soups or sauces thickened with wheat flour (swap for cornstarch or rice flour)
- Processed meats like sausages or burgers (look for gluten-free labels)
If you suspect gluten is affecting you, try a short elimination period of about four weeks. Track your symptoms to see whether your skin or joints feel better.
Dairy Products and Inflammatory Proteins in Psoriasis
Dairy can be complicated. Some people tolerate it well, while others notice more flares when they consume it regularly. The main issue comes from two proteins: casein and whey, which can trigger inflammation in sensitive individuals.
If you want to test your response, try reducing or eliminating cow’s milk products for a few weeks. Some people find that goat or sheep dairy, which contains a different type of casein, is easier on the body. Pay close attention to how your skin and joints respond so you can decide what works best for you.
Nightshade Vegetables and Psoriatic Arthritis Flare-Ups
Nightshades are a group of vegetables that include tomatoes, potatoes, eggplants, and peppers. They contain a compound called solanine, which may trigger inflammation in some people. Not everyone reacts to nightshades, but if you notice your joints or scalp symptoms get worse after eating them, it may be worth trying a short elimination to see if things improve.
Alcohol and Its Inflammatory Effects on Psoriasis and Arthritis
Alcohol may feel relaxing in the moment, but it can actually worsen both scalp psoriasis and psoriatic arthritis. It stresses your liver, fuels inflammation, and may interfere with certain medications. If you notice flare-ups after drinking, try replacing alcohol with gentler alternatives like sparkling water, lemon water, or calming herbal teas.

Healing Foods for Scalp Psoriasis and Psoriatic Arthritis
Alcohol may feel relaxing in the moment, but it can actually worsen both scalp psoriasis and psoriatic arthritis. It stresses your liver, fuels inflammation, and may interfere with certain medications. If you notice flare-ups after drinking, try replacing alcohol with gentler alternatives like sparkling water, lemon water, or calming herbal teas.
Omega-3 Rich Fish and Healthy Fats for Psoriatic Arthritis Relief
Omega-3 fatty acids are powerful when it comes to reducing inflammation. They help lower the activity of inflammatory chemicals in the body, which means fewer flare-ups and less joint stiffness.
Best sources of omega-3s include:
- Fatty fish such as salmon, sardines, mackerel, and herring
- Plant-based options like flaxseeds, chia seeds, and walnuts
Aim for at least two servings of oily fish each week. If you follow a plant-based diet, try adding ground flaxseed or chia seeds to smoothies or oatmeal for a daily boost.
Colorful Antioxidant-Rich Vegetables That Heal Psoriasis Naturally
Vegetables are packed with antioxidants, which protect your cells from oxidative stress. That stress can trigger inflammation and worsen both psoriasis and arthritis. Each color in vegetables represents different protective compounds, so variety is key.
Examples:
- Leafy greens such as spinach and kale are rich in vitamin E, which supports skin repair
- Orange vegetables like carrots and sweet potatoes provide beta-carotene, which can reduce inflammation
- Cruciferous vegetables such as broccoli and Brussels sprouts contain sulforaphane, a compound linked to lower inflammation
Try to fill half your plate with a mix of colors at every meal.
Anti-Inflammatory Spices and Herbs for Joint and Skin Health
Your spice rack can do more than flavor your meals. Certain herbs and spices have compounds that naturally calm inflammation.
Top choices:
- Turmeric: contains curcumin, which may help ease skin and joint flare-ups
- Ginger: supports digestion and helps reduce inflammatory signals
- Garlic: provides allicin, which helps balance the immune system
Sprinkle these into soups, stews, stir-fries, or smoothies to make them part of your daily routine.

Probiotic Foods for Gut Health, Psoriasis, and Arthritis
Your gut health plays an important role in how your immune system functions. A balanced gut can help lower inflammation signals that affect both skin and joints. Adding probiotic foods is an easy way to support this balance.
Good sources include:
- Unsweetened live yogurt
- Kefir
- Fermented vegetables like sauerkraut and kimchi
Start with small portions and notice how your body responds.

Fiber-Rich Whole Grains to Reduce Inflammation
Whole grains are very different from refined grains. They provide fiber, which supports gut health and helps regulate blood sugar levels. Both of these are important for keeping inflammation under control.
Better grain choices:
- Quinoa
- Brown rice
- Oats
- Barley
- Bulgur
Choose whole grains that you tolerate well, and try to make them a quarter of your plate.
Sample 7-Day Anti-Inflammatory Diet Plan for Psoriasis and Arthritis
Starting an anti-inflammatory diet can feel overwhelming at first, but having a simple plan makes it easier. Think of this as a guide to help you build meals that calm inflammation, support scalp and joint health, and keep you satisfied. You can adjust portion sizes to your needs and swap in foods you prefer as long as they fit the anti-inflammatory framework.

Day 1
- Breakfast: Overnight oats with chia seeds, blueberries, and almond butter
- Lunch: Quinoa salad with chickpeas, cucumber, tomato, and olive oil dressing
- Dinner: Grilled salmon with roasted broccoli and sweet potato
- Snack: Handful of walnuts or carrot sticks with hummus
Day 2
- Breakfast: Smoothie with spinach, banana, flaxseed, and plant-based milk
- Lunch: Brown rice bowl with roasted vegetables and turmeric-spiced chicken
- Dinner: Lentil soup with a side of leafy green salad
- Snack: Greek yogurt with a spoon of sauerkraut on the side
Day 3
- Breakfast: Scrambled eggs with spinach and avocado
- Lunch: Sardine salad with leafy greens, olive oil, and lemon
- Dinner: Baked cod with quinoa and steamed asparagus
- Snack: Apple slices with almond butter
Day 4
- Breakfast: Chia pudding topped with raspberries and walnuts
- Lunch: Whole grain wrap with grilled vegetables and hummus
- Dinner: Turkey chili made with beans and anti-inflammatory spices like cumin and garlic
- Snack: Small bowl of kefir with berries
Day 5
- Breakfast: Oatmeal with cinnamon, banana, and chia seeds
- Lunch: Salmon burger served on a lettuce wrap with side salad
- Dinner: Stir-fried tofu with broccoli, bell peppers, and ginger
- Snack: Handful of pumpkin seeds
Day 6
- Breakfast: Smoothie bowl with mixed berries, ground flaxseed, and coconut flakes
- Lunch: Quinoa and black bean salad with avocado and lime
- Dinner: Grilled mackerel with roasted Brussels sprouts and sweet potato mash
- Snack: Carrot and cucumber sticks with tahini dip
Day 7
- Breakfast: Scrambled eggs with sautéed kale and garlic
- Lunch: Brown rice with salmon sashimi and seaweed salad
- Dinner: Lentil and vegetable stew with turmeric and ginger
- Snack: A pear with a few walnuts
Pro tip: Prep ingredients in batches. Roast vegetables ahead of time, cook a pot of quinoa, or make overnight oats for quick grab-and-go meals. Planning ahead makes it easier to stick to your anti-inflammatory routine without stress.
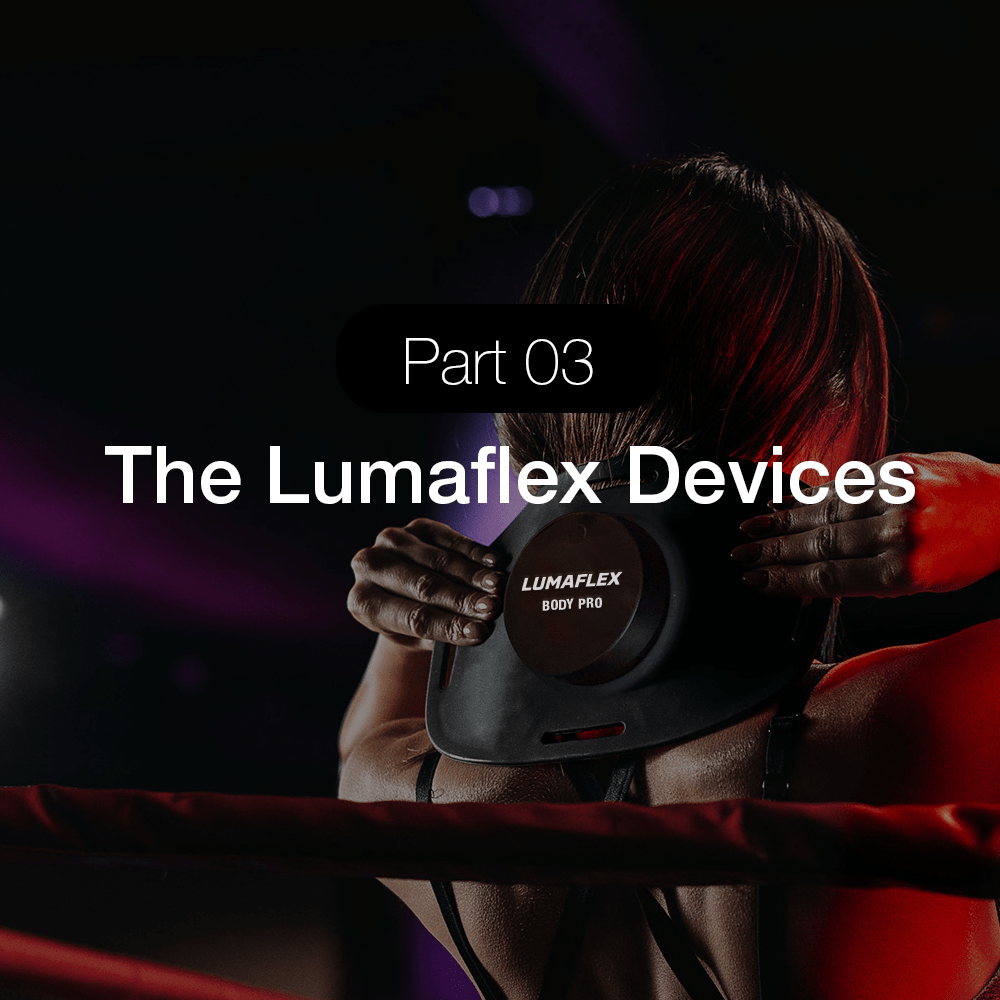
Complementary Treatment: Red Light Therapy for Psoriasis and Psoriatic Arthritis with Lumaflex
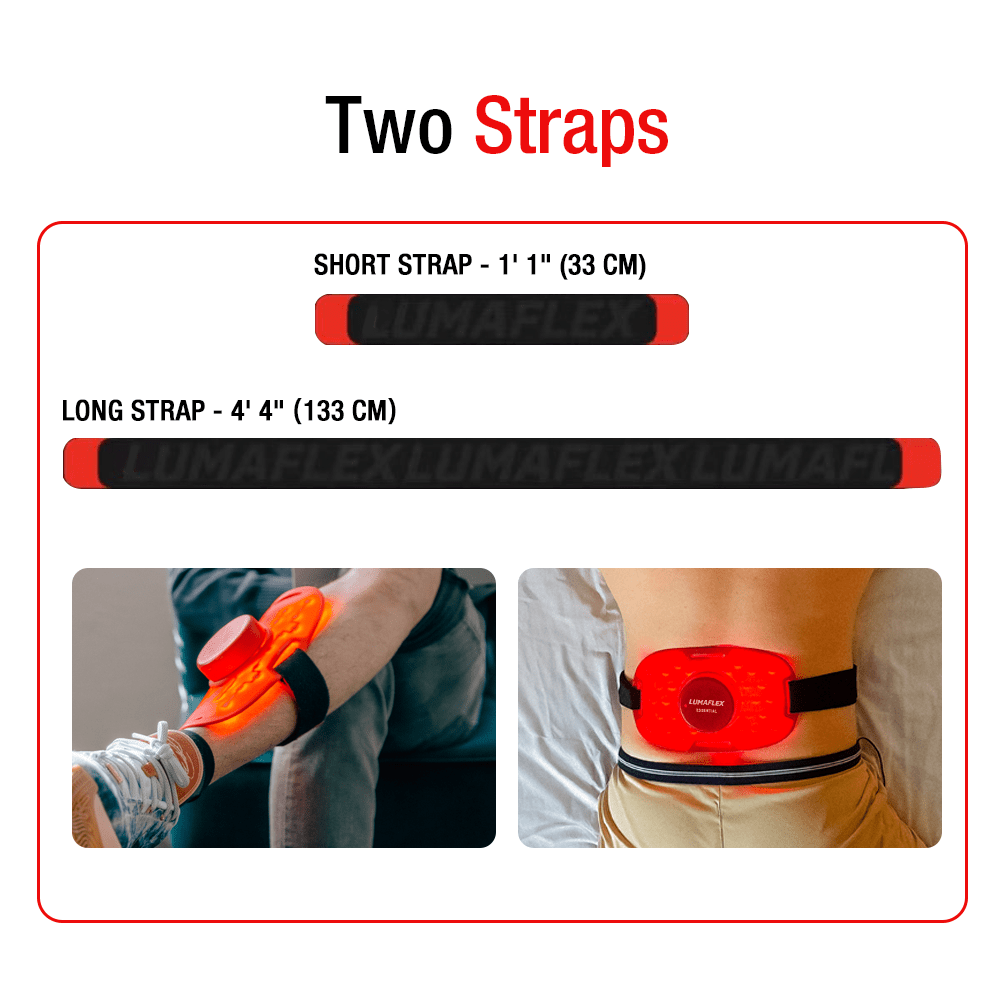
Diet is one of your most powerful tools for calming psoriasis and psoriatic arthritis, but sometimes you need an extra layer of support. That is where red light therapy comes in.
Research shows that red light therapy uses gentle, low-level wavelengths of light to calm inflammation under the skin. This type of light can help reduce scalp plaques, ease itching, and even relieve some of the stiffness and discomfort that comes with psoriatic arthritis.
What makes red light therapy so appealing is that it is non-invasive and safe for regular use. With a device like Lumaflex, you can use it at home whenever it fits your schedule, rather than having to book repeated clinic appointments. Many people find it helpful as part of their self-care routine, especially when combined with an anti-inflammatory diet.
Think of it this way: food works from the inside to calm inflammation, and red light therapy works from the outside to soothe skin and joints. When you pair them together, you give your body a stronger foundation for healing.

What the Research Says About Red Light Therapy
You might be wondering, “Does this really work?” The good news is that there is growing research behind red light therapy for psoriasis and arthritis symptoms.
- A study published in Frontiers in Photonics found that red light therapy can modulate nitric oxide homeostasis, with implications for the phototherapy of psoriasis.
- Some small trials have also reported improvements in joint pain and stiffness for people with psoriatic arthritis after consistent use of low-level light therapy.
- While more large-scale studies are still needed, the early evidence suggests that this treatment is safe, well tolerated, and a helpful add-on to your regular care plan.
The takeaway: red light therapy is not a cure, but it may help reduce flare-ups and give you another tool for managing your symptoms alongside diet and medical treatment.
If you are curious about trying red light therapy at home, Lumaflex makes it simple. It is non-invasive, easy to use, and can be part of your daily routine alongside your anti-inflammatory diet.
Practical Tips for Starting a Psoriatic Arthritis and Psoriasis Diet
Making changes to your diet and lifestyle can feel overwhelming at first, but it does not have to be. The best results usually come from small, steady steps that add up over time. Here are some ways to get started:
Start with one swap at a time. Instead of cutting out everything at once, focus on one easy change. For example, replace your afternoon soda with sparkling water and lemon, or swap white bread for quinoa or brown rice. Small wins build confidence.
Track your meals and symptoms. Keeping a simple journal or using a tracking app can help you notice patterns. If your joints feel stiffer after pasta, or your scalp flares up after ice cream, you will have a clearer picture of what is happening.
Plan ahead for success. Batch-cook grains, wash and chop vegetables, and keep healthy snacks like nuts or fruit ready to go. Having nourishing foods within reach makes it easier to stick with your plan, especially on busy days.
Work with your healthcare team. Every body is different. A dietitian can help tailor your meals to your needs, and your dermatologist or rheumatologist can guide you on safe ways to combine diet, medications, and complementary treatments.
Most importantly, remember that consistency is what makes the difference. Think of these changes as long-term habits rather than a short-term diet. Each choice you make to lower inflammation is a step toward calmer skin and more comfortable joints.

Conclusion – Managing Scalp Psoriasis and Psoriatic Arthritis with a Holistic Approach
Managing scalp psoriasis and psoriatic arthritis takes patience, but you are not powerless. The choices you make each day can help calm inflammation and support healing. By focusing on anti-inflammatory foods like colorful vegetables, omega-3 rich fish, whole grains, and healthy fats, while easing away from sugar, processed foods, high-fat dairy, and alcohol, you give your body a stronger foundation to heal.
Remember, this is not about being perfect. It is about consistency. Even small steps, like swapping one meal or adding more greens to your plate, can make a difference over time. Pairing your diet with supportive treatments such as red light therapy, stress relief practices, and gentle skincare gives you a well-rounded plan for managing flare-ups.
You deserve to feel better in your skin and joints. With steady effort and the right tools, you can move toward more comfort, fewer flares, and a lifestyle that supports your long-term health.
Along with food and lifestyle shifts, tools like red light therapy can give you extra support. If you want an at-home option that helps calm skin and joints, Lumaflex may be worth exploring.
FAQ – Scalp Psoriasis and Psoriatic Arthritis Diet (Foods That Heal vs. Trigger)
What diet is best for scalp psoriasis?
The most supportive diet is one that reduces inflammation. This usually means focusing on whole, nutrient-dense foods: plenty of colorful vegetables, omega-3 rich fish, whole grains, legumes, nuts, seeds, and healthy fats like olive oil or avocado. Many people also benefit from limiting processed foods, sugar, alcohol, and sometimes gluten or dairy if they notice those trigger flare-ups.
What foods trigger psoriatic arthritis flare-ups?
Common culprits include refined sugar, processed foods, alcohol, fried foods, high-fat dairy, and sometimes gluten or nightshade vegetables like tomatoes, peppers, and potatoes. Triggers can be different for each person, so keeping track of what you eat and how you feel is the best way to uncover your own patterns.
Should I avoid eggs if I have psoriasis?
Not everyone with psoriasis reacts to eggs, but some people do find that they worsen inflammation or skin irritation. If you are unsure, try keeping a food journal and tracking symptoms when you eat eggs. If you notice a connection, you could experiment with an egg-free trial for a few weeks to see if your scalp or joint symptoms improve.
Can scalp psoriasis be caused by diet?
Diet does not directly cause scalp psoriasis since it is an autoimmune condition, but what you eat can strongly influence flare-ups. Pro-inflammatory foods can make symptoms worse, while an anti-inflammatory diet can help reduce irritation and support skin healing. In other words, diet is not the root cause, but it is a powerful lever for symptom management.
How does diet affect scalp psoriasis and psoriatic arthritis?
Your diet can either calm or fuel inflammation, which is at the root of both conditions. When you fill your plate with anti-inflammatory foods like vegetables, fruits, healthy fats, and omega-3 rich fish, you give your body tools to soothe skin flare-ups and ease joint stiffness. On the other hand, foods like sugar, alcohol, and heavily processed snacks can act like fuel for the fire, making symptoms worse.
Can gluten make psoriasis worse?
For some people, yes. Even without celiac disease, gluten can trigger inflammation and lead to flare-ups in the skin or joints. About one in four people with psoriatic disease are sensitive to gluten. If you suspect it may be affecting you, try a short gluten-free trial (ideally with your doctor’s guidance) and track whether your symptoms improve.
Should I combine diet with other treatments?
Absolutely. Food is a powerful foundation, but it works best when combined with other approaches. Many people find better relief when they pair an anti-inflammatory diet with treatments their doctor prescribes, stress management strategies like yoga or meditation, gentle skincare, and supportive therapies such as red light therapy. Think of it as building a toolbox. Each piece works better together.
Related Readings
- What is Biohacking Diet? Why 80% of Health Enthusiasts Are Ditching Traditional Diets
- Red Light Therapy for Head Health: Daily Routine Tips and Tricks
- Red Light Therapy for Skin, Pain, and Hair: How Long Will It Take to Notice Changes?
- Red Light Therapy Results for Skin: Complete Benefits Guide
- Red Light Therapy 101: Everything You Need to Know
- Red Light Therapy for Pain 101: Benefits and How It Works
- A Meta-analysis: Red Light Therapy at 630nm for Chronic Pain
- How Light Therapy Can Alleviate Arthritis Pain
- Everything About Red Light Therapy for Hair Loss
- Estrogen and Hair Loss: Red Light Therapy for Scalp Revival