A Meta-analysis: Red Light Therapy for Dogs

Red light therapy, also known as photobiomodulation therapy (PBMT), has emerged as one of the fastest-growing treatment modalities in veterinary medicine, with approximately 20% of veterinary clinics now offering this non-invasive therapeutic option. The therapy uses specific wavelengths of red and near-infrared light to stimulate cellular processes, particularly ATP production in mitochondria, leading to enhanced healing, pain reduction, and inflammation control.
Table of content
- 1. Scientific evidence shows promising but limited support for canine applications
- 2. Safety profile demonstrates excellent tolerability with minimal contraindications
- 3. Multiple conditions benefit from targeted photobiomodulation protocols
- 4. Device landscape offers comprehensive options from consumer to professional grade
- 5. Veterinary professionals increasingly recommend integration with conventional treatments
- 6. Treatment protocols vary by condition but follow established dosimetry principles
- 7. Economic analysis reveals substantial cost advantages for chronic conditions
- 8. Comparison to other therapies reveals synergistic rather than competitive positioning
- 9. Regulatory environment facilitates accessibility while creating quality challenges
- 10. Future outlook
- 11. References
Scientific evidence shows promising but limited support for canine applications
The research base for red light therapy in dogs is characterized by moderate evidence for osteoarthritis management and emerging evidence for other conditions, though study quality varies significantly. The strongest clinical evidence comes from controlled trials examining joint disease treatments.
Osteoarthritis represents the most compelling application, with multiple randomized controlled trials demonstrating substantial benefits. In a pivotal study by Looney et al. (2018), 82% of dogs with elbow osteoarthritis achieved at least 50% reduction in NSAID medication requirements compared to zero percent in the control group. The study also showed significant improvements in nine out of eleven measured pain parameters. Similarly, research by Alves et al. (2022) found PBMT reduced pain levels and improved clinical findings compared to meloxicam treatment, while Barale et al. (2023) documented increased daily activity levels from 93,481 steps at baseline to 179,309 steps at six weeks.
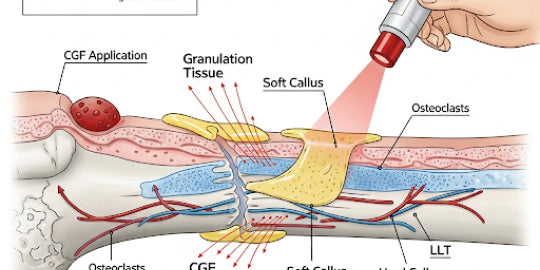
Wound healing applications show mixed but generally positive results. Studies demonstrate accelerated tissue repair through enhanced collagen synthesis and improved angiogenesis. Mississippi State University research on dachshunds showed significantly faster healing and improved cosmetic appearance of surgical incisions, with full-thickness wounds healing completely in 21 days rather than conventional recovery times. However, post-surgical pain management studies have produced conflicting results, with some showing improved recovery while others found no significant benefits.
Dermatological conditions represent an area with limited high-quality evidence. While multiple studies exist, only three out of 19 dermatological studies met criteria for conclusive evidence. Fluorescence biomodulation showed effectiveness for canine interdigital pyoderma, and low-level laser therapy proved beneficial for sterile pyogranulomatous pododermatitis.
The research reveals critical limitations including small sample sizes (most studies n<25), heterogeneous protocols with wide variation in wavelengths and doses, lack of standardized parameters, and potential publication bias due to industry funding. Future research priorities include large-scale multi-center trials, standardized dosimetry protocols, and long-term efficacy studies exceeding one year.
Safety profile demonstrates excellent tolerability with minimal contraindications
Red light therapy presents a remarkably favorable safety profile when administered appropriately under veterinary guidance. Multiple studies consistently report that the therapy is "well-tolerated by animals with few, if any, side effects." A comprehensive 2023 systematic review evaluating 45 articles found minimal adverse effects reported across experimental and clinical studies.
Documented side effects are rare and mild, including occasional slight skin irritation or temporary redness at treatment sites in sensitive animals. No systemic adverse events have been reported in peer-reviewed veterinary studies. The therapy's non-invasive nature eliminates risks associated with anesthesia or surgical interventions.
Absolute contraindications include direct eye exposure (retinal damage is the primary safety concern) and active malignancies without direct veterinary supervision due to theoretical tumor growth stimulation concerns. Relative contraindications encompass pregnancy (limited safety data), seizure disorders, and photosensitivity conditions. Safety precautions require protective eyewear for handlers, removal of metallic collars or tags, and proper dosing to avoid diminished results or potential tissue damage.
Professional veterinary organizations increasingly embrace the therapy, with professional guidelines being published for standardized treatments. The veterinary profession views red light therapy as a safe, effective, and simple way to enhance companion animal health, though emphasizing the importance of proper training, protocols, and integration into comprehensive treatment plans.
Multiple conditions benefit from targeted photobiomodulation protocols
Red light therapy demonstrates efficacy across a broad spectrum of canine health conditions, with treatment protocols varying by application and severity.
Joint and musculoskeletal conditions show the strongest clinical response. Arthritis protocols typically use 8-12 J/cm² for most joints, with higher doses (10-20 J/cm²) required for elbow joints. Initial treatment phases involve 2-3 sessions per week for 4-6 weeks, transitioning to maintenance sessions spaced further apart based on patient response. Session duration ranges from 5 minutes per joint to 10-15 minutes for larger areas.
Wound healing applications utilize 1-10 J/cm² depending on wound depth and severity. Acute wounds receive daily treatments for 5-7 sessions, while chronic wounds require 3-5 treatments per week until healing. Wavelength selection depends on tissue depth: 630nm for superficial wounds, 660nm and 850nm for deeper tissue involvement. Treatment duration spans 1-5 minutes for small wounds and up to 10 minutes for larger areas.
Post-surgical recovery protocols begin within 24-48 hours after surgery with daily treatments for 3-5 days initially, then tapering based on healing response. Research shows dogs receiving post-operative PBMT demonstrate faster return to ambulation, reduced pain scores, and increased proportion resuming normal eating patterns compared to controls.
Additional conditions with documented benefits include neurological conditions (intervertebral disc disease, degenerative myelopathy, cognitive dysfunction), chronic diarrhea, gingivitis, ear infections, and snake bite envenomation. Each condition requires specific protocols optimized for tissue type, penetration depth requirements, and healing objectives.
Device landscape offers comprehensive options from consumer to professional grade
The veterinary red light therapy market provides diverse technological solutions ranging from consumer-friendly LED panels to professional-grade Class IV laser systems, each with distinct advantages and applications.
Professional veterinary equipment features Class IV laser systems exceeding 500mW output power, species-specific protocols for different animals, advanced software with treatment tracking capabilities, multiple wavelength options (typically 660nm, 810nm, 830nm, 850nm), and clinical-grade build quality. Professional systems cost $15,000-$45,000 and include comprehensive training and service support. Leading manufacturers include Companion Animal Health (LiteCure), K-Laser (ASA Srl), Multi Radiance Medical, and SpectraVET.
Consumer and home devices utilize LED or low-power laser technology with preset treatment modes, battery operation, simplified controls, and safety-focused design. These handheld and panel systems cost $200-$3,000 and provide accessible treatment options for pet owners. Categories include handheld devices, panel systems for broad coverage, flexible pad/wrap systems for joint-specific applications, and professional cart systems for clinical use.
LED versus laser technology comparison reveals important distinctions. LEDs offer eye-safe operation without protective eyewear requirements, no heat generation, broader wavelength spectrum, lower cost, longer device lifespan, and suitability for home use with larger treatment areas. However, they provide less focused beams, lower power density, longer treatment times, and limited penetration depth compared to lasers.
Laser technology advantages include precise focused beam delivery, higher power density, faster treatment times, deeper tissue penetration (5-6cm depth versus 2-3cm for LEDs), more targeted therapy, and professional-grade results. Disadvantages encompass requirements for eye protection, professional supervision recommendations, higher cost, heat generation potential, safety training needs, and smaller treatment areas per application.
Key wavelengths and specifications center around 660nm (red light) for surface treatments and superficial tissue applications, and 850nm (near-infrared) for deepest penetration targeting mitochondria effectively in joints and deep tissue. Professional devices offer 1W to 60W+ power output, while consumer devices range from 5mW to 500mW.
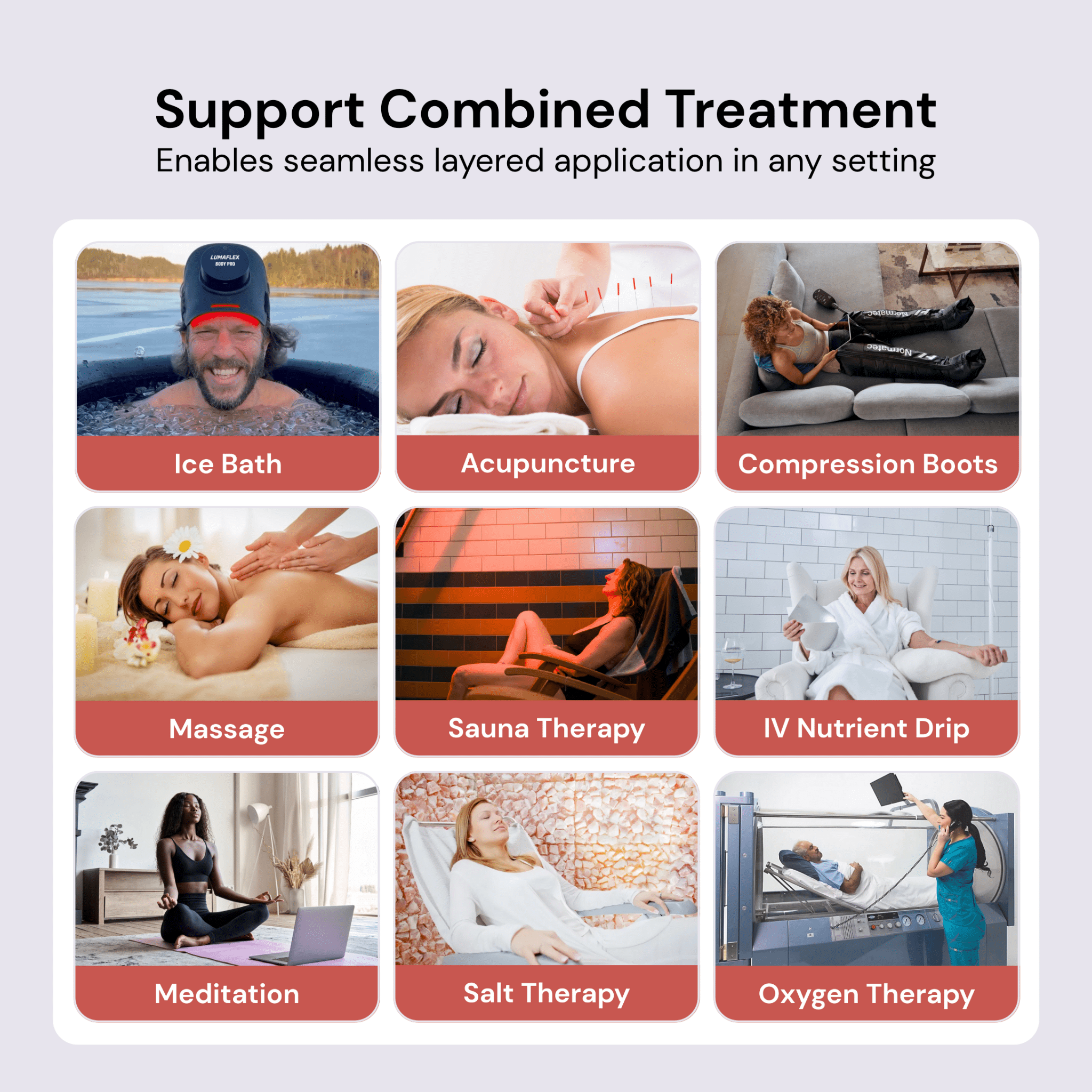
Veterinary professionals increasingly recommend integration with conventional treatments
Professional adoption accelerates rapidly with red light therapy representing one of the fastest-growing treatment modalities in American veterinary practice. Professional veterinary perspectives emphasize the therapy's value as a complementary rather than replacement treatment, working synergistically with conventional therapies to enhance outcomes while potentially reducing medication requirements.
Expert veterinarian opinions highlight both promise and limitations. Dr. Laurie Brush notes that "red light therapy offers a non-invasive, drug-free treatment option with promising medical benefits for managing pain, enhancing orthopedic health, and improving quality of life." However, Dr. Nina Kieves from Ohio State University cautions that "the literature on laser therapy is currently limited" with studies having "small sample sizes, lack control groups, and vary in protocols."
Professional recommendations consistently emphasize veterinary supervision as essential, individual patient assessment for treatment appropriateness, integration into multimodal treatment plans rather than standalone therapy, and regular veterinary reassessment to monitor effectiveness and adjust treatments. Professional training requirements focus on proper device operation, safety protocols, dosing optimization, and patient monitoring techniques.
Clinical integration best practices include staff training for proper dosing and safety protocols, individualized treatment protocols based on patient size and condition, comprehensive documentation tracking treatment parameters and patient responses, and multimodal approaches combining red light therapy with conventional treatments for optimal results.
Treatment protocols vary by condition but follow established dosimetry principles
Standardized protocols emerge from clinical research despite some variation in specific parameters. The traditional "3-2-1" protocol (three treatments first week, two treatments second week, one treatment third week) has evolved toward more individualized approaches based on condition acuity and patient response.
Acute conditions typically require daily treatments initially, then every other day as improvement occurs. Chronic conditions benefit from 2-3 times per week initially, then maintenance sessions monthly or as needed. Post-surgical applications involve 3-7 consecutive daily treatments for optimal healing support.
Dosimetry guidelines recommend 0.1-6 J/cm² for cellular benefits, with most studies using 3-10 J/cm². Power density generally ranges 50-200 mW/cm² at tissue surface with contact or near-contact application for maximum energy delivery. Treatment area considerations account for fur density (often requiring clipping), patient comfort, and tissue penetration requirements.
Session duration parameters span 1-3 minutes for small wounds, 3-10 minutes per joint for musculoskeletal treatments, 10-20 minutes for large areas using scanning techniques, and up to 30 minutes total session time for multiple treatment sites. Treatment course length varies from 5-10 sessions for acute injuries to 6-12 sessions initially with maintenance for chronic conditions.
Economic analysis reveals substantial cost advantages for chronic conditions
Professional treatment costs range $30-$100 per session with typical regimens requiring 2-3 sessions per week over 6-12 weeks, resulting in total professional treatment costs of $360-$3,600 per condition. Package deals offer 20-30% discounts with 10-session packages typically costing $400-$800.
Home device economics demonstrate compelling cost-effectiveness, particularly for chronic conditions. Device costs range from $200-$500 for handheld units to $800-$1,500 for professional-grade home systems. The break-even point occurs after 4-8 professional sessions, with home devices providing "thousands of treatments" per device purchase.
Comparative economic analysis shows red light therapy provides 10-20x cost advantages over traditional laser therapy, with professional laser treatments costing $50-$100 per session and equipment costing "several thousand dollars" compared to red light devices starting at "couple hundred dollars."
Insurance coverage remains limited but growing with some pet insurance policies covering red light therapy when veterinarian-recommended. Healthy Paws Pet Insurance covers treatments performed by licensed veterinarians for non-pre-existing conditions, while Embrace Pet Insurance includes complementary treatment coverage at no additional cost. Coverage typically requires documentation of medical necessity and professional administration, with home devices generally not covered.
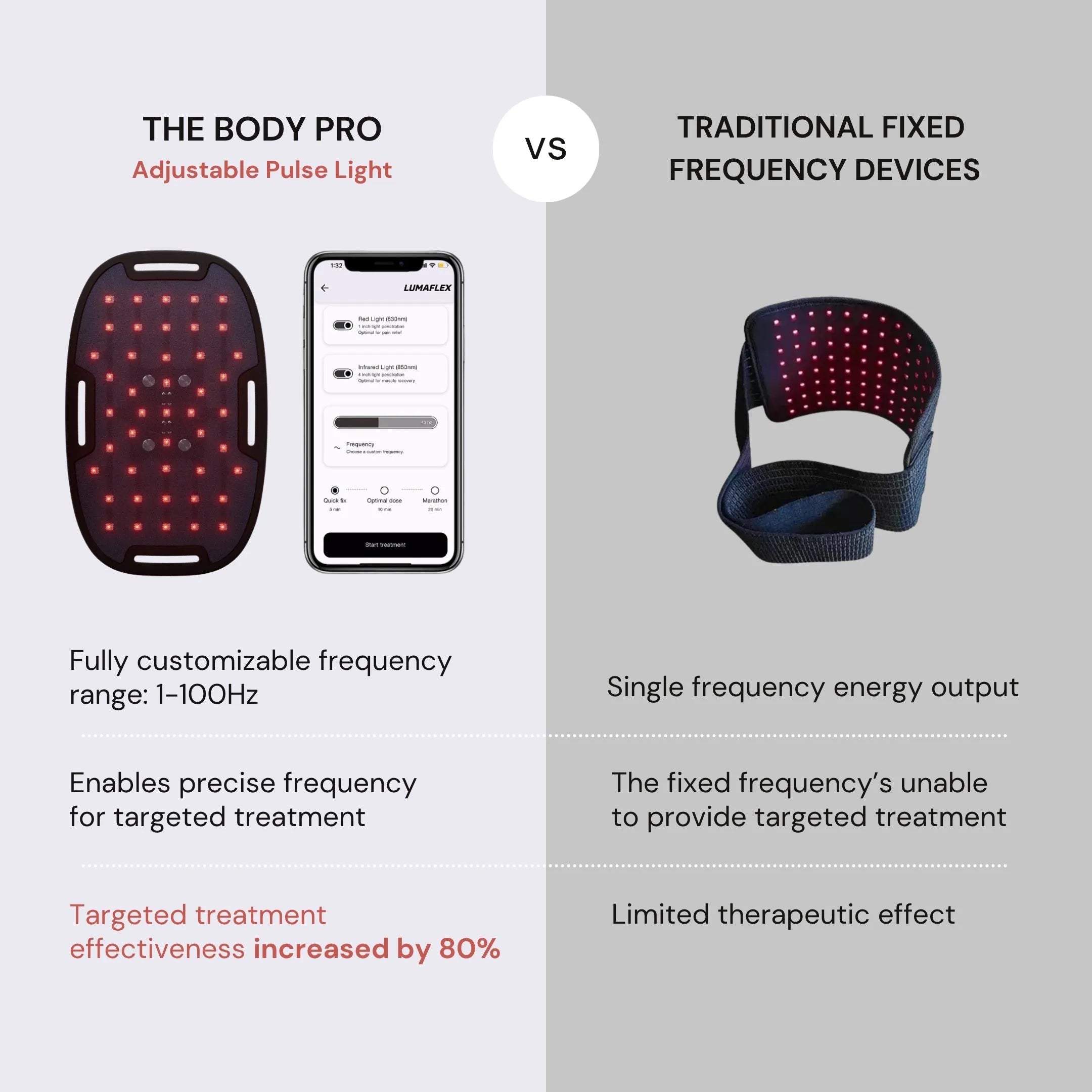
The Lumaflex Body Pro uses red light wavelength 630nm + infrared wavelength 850nm to support pets' pain management. It is a comprehensive, reliable, and effective solution with 10 international quality certifications and 9 design awards.
Comparison to other therapies reveals synergistic rather than competitive positioning
Red light therapy occupies a unique niche in the veterinary treatment ecosystem as a complementary modality that enhances rather than replaces conventional treatments. Clinical studies demonstrate significant drug-sparing effects, with 82% of dogs in arthritis studies achieving 50% or greater reduction in NSAID medication requirements.
Comparison to pharmaceutical interventions reveals red light therapy's advantage in avoiding gastrointestinal and organ risks associated with long-term NSAID use. While NSAIDs cost $30-$100+ monthly for chronic conditions and carry liver, kidney, and stomach complication risks, red light therapy provides medication reduction benefits with minimal side effects.
Physical therapy comparison shows complementary rather than competitive relationship. Physical therapy costs $50-$150 per session with well-established effectiveness for mobility and recovery, but requires specialized facilities and trained therapists. Red light therapy often integrates synergistically with physical therapy protocols to enhance outcomes.
Hydrotherapy applications primarily target mobility and joint conditions at $40-$80 per session but require facility access and aren't suitable for all conditions. Acupuncture costs $60-$120 per session with good insurance coverage but requires licensed veterinary practitioners. Red light therapy's advantages include multi-condition applicability with single devices, no sedation or restraint requirements, and broad accessibility.
Therapeutic positioning analysis confirms red light therapy's role as a complementary therapy working synergistically with other treatments, providing drug-sparing effects to reduce medication requirements, offering non-invasive treatment without sedation needs, and enabling multi-condition treatment with single devices.
Regulatory environment facilitates accessibility while creating quality challenges
FDA oversight of veterinary red light devices remains minimal, with no pre-market approval requirements, mandatory establishment registration, device listing requirements, or post-market surveillance reporting. Unlike human medical devices requiring 510(k) premarket notifications, veterinary devices operate under manufacturer self-regulation with responsibility for ensuring devices are "safe, effective, and properly labeled."
Current regulatory framework imposes minimal regulatory burden with no device classification system, mandatory design controls, quality system regulations, or clinical trial requirements. FDA enforcement authority allows action against misbranded or adulterated devices through voluntary adverse event reporting, but shows limited historical enforcement activity.
Regulatory implications create potential for inconsistent device quality, no standardized efficacy requirements, reliance on manufacturer self-compliance, and limited post-market surveillance. This regulatory environment facilitates market accessibility and innovation but creates quality assurance challenges that market forces and professional standards must address.
Market accessibility benefits from widespread availability through major retailers, direct-to-consumer sales channels, international shipping options, and multiple price points. The global veterinary equipment market valued at $2.96 billion in 2025 grows at 7.80% CAGR, with red light therapy representing one of the fastest-growing segments, particularly in the Asia-Pacific region.
Future outlook
The convergence of scientific validation, economic advantages, and professional acceptance positions red light therapy for continued growth in veterinary medicine. Market trends indicate increasing shift toward home-based therapy devices, enhanced integration of telemedicine and remote monitoring, improved safety features for consumer devices, and cost reduction making professional-grade technology more accessible.
Research priorities focus on large-scale standardized trials with longer follow-up periods, dose-response relationship characterization, personalized protocols based on patient characteristics, biomarker-guided treatment optimization, and combination therapy protocol development. Regulatory evolution may include increased oversight as the market matures, though current minimal barriers support innovation and accessibility.
Professional integration will likely expand through enhanced training and certification programs, standardized treatment protocol development, improved insurance coverage recognition, and strengthened evidence-based practice guidelines. The therapy's positioning as a safe, effective, economical complementary treatment option ensures its continued relevance in evolving veterinary care paradigms.
Red light therapy for dogs represents a mature emerging technology with solid scientific foundations, excellent safety profiles, significant economic advantages, and growing professional acceptance. While research gaps remain and regulatory oversight continues evolving, the therapy's demonstrated benefits for pain management, wound healing, and chronic condition support establish it as a valuable component of comprehensive veterinary care.
References
- Millis DL, Bergh A. A Systematic Literature Review of Complementary and Alternative Veterinary Medicine: Laser Therapy. Animals (Basel). 2023 Feb 14;13(4):667. doi: 10.3390/ani13040667. PMID: 36830454; PMCID: PMC9951699.
- Alves JC, Santos A, Jorge P, Carreira LM. A randomized double-blinded controlled trial on the effects of photobiomodulation therapy in dogs with osteoarthritis. Am J Vet Res. 2022 Jun 28;83(8):ajvr.22.03.0036. doi: 10.2460/ajvr.22.03.0036. PMID: 35895799.
- Bennaim M, Porato M, Jarleton A, Hamon M, Carroll JD, Gommeren K, Balligand M. Preliminary evaluation of the effects of photobiomodulation therapy and physical rehabilitation on early postoperative recovery of dogs undergoing hemilaminectomy for treatment of thoracolumbar intervertebral disk disease. Am J Vet Res. 2017 Feb;78(2):195-206. doi: 10.2460/ajvr.78.2.195. PMID: 28140641.
- Perego R, Proverbio D, Zuccaro A, Spada E. Low-level laser therapy: Case-control study in dogs with sterile pyogranulomatous pododermatitis. Vet World. 2016 Aug;9(8):882-7. doi: 10.14202/vetworld.2016.882-887. Epub 2016 Aug 22. PMID: 27651678; PMCID: PMC5021839.
- Perego R, Mazzeo M, Spada E, Proverbio D. Critically Appraised Topic on Low-Level Laser Therapy (LLLT) in Dogs: An Advisable Treatment for Skin Diseases? Vet Sci. 2022 Sep 14;9(9):505. doi: 10.3390/vetsci9090505. PMID: 36136721; PMCID: PMC9502196.
- Looney AL, Huntingford JL, Blaeser LL, Mann S. A randomized blind placebo-controlled trial investigating the effects of photobiomodulation therapy (PBMT) on canine elbow osteoarthritis. Can Vet J. 2018 Sep;59(9):959-966. PMID: 30197438; PMCID: PMC6091142.
- Dewey CW, Rishniw M, Brunke MW, Gerardi J, Sakovitch K. Transcranial photobiomodulation therapy improves cognitive test scores in dogs with presumptive canine cognitive dysfunction: A case series of five dogs. Open Vet J. 2024 May;14(5):1167-1171. doi: 10.5455/OVJ.2024.v14.i5.11. Epub 2024 May 31. PMID: 38938435; PMCID: PMC11199766.
- Miller LA, Torraca DG, De Taboada L. Retrospective Observational Study and Analysis of Two Different Photobiomodulation Therapy Protocols Combined with Rehabilitation Therapy as Therapeutic Interventions for Canine Degenerative Myelopathy. Photobiomodul Photomed Laser Surg. 2020 Apr;38(4):195-205. doi: 10.1089/photob.2019.4723. PMID: 32301669; PMCID: PMC7187977.
- How FDA Regulates Animal Devices - FDA
- Special Considerations for 510(k)s - FDA
- Randa Zein, Wayne Selting, Michael R. Hamblin, "Review of light parameters and photobiomodulation efficacy: dive into complexity," J. Biomed. Opt. 23(12) 120901 (11 December 2018) https://doi.org/10.1117/1.JBO.23.12.120901